Immunotherapy gives hope for 'incurable' prostate cancer
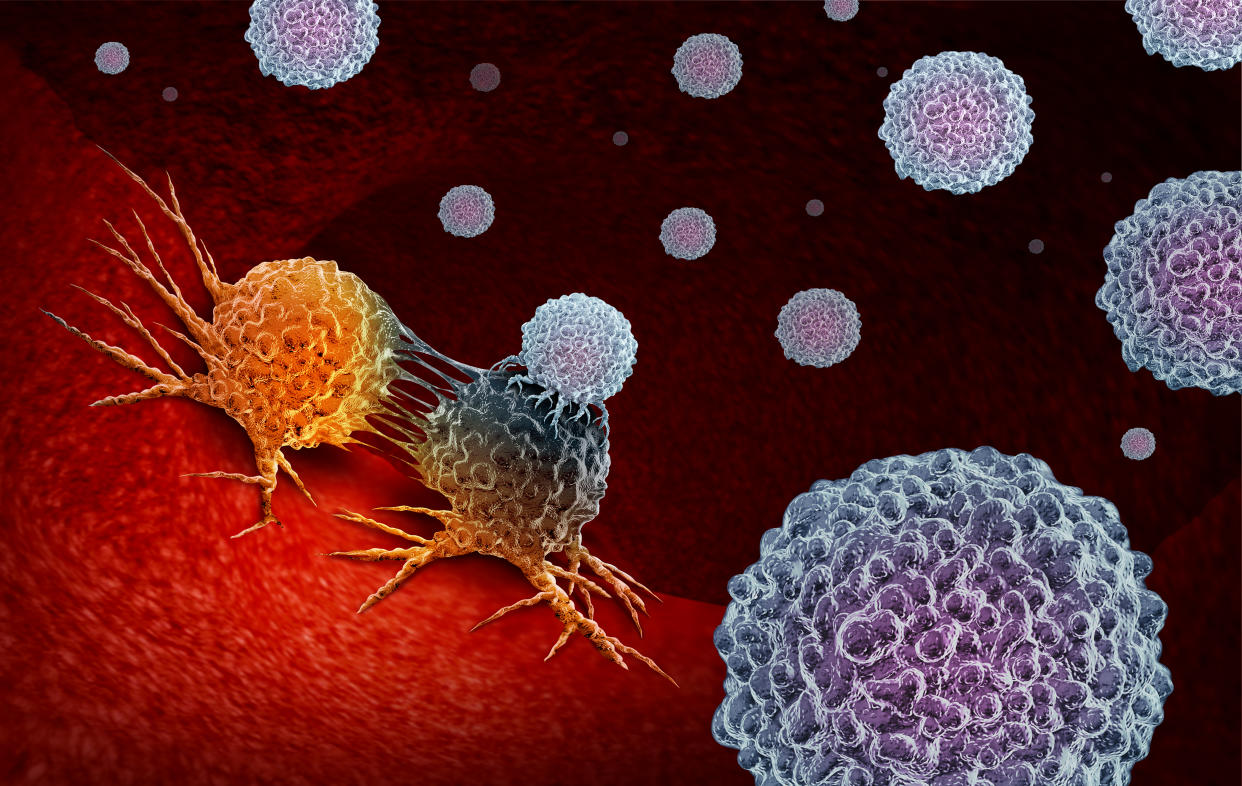
Immunotherapy could offer new hope for men with “incurable” prostate cancer, research suggests.
UK scientists looked at 258 patients who had exhausted all treatment options.
READ MORE: Rod Stewart tells men to check for prostate cancer, here’s what you need to know
The men were given the IV drug pembrolizumab, brand name Keytruda, which works with the immune system to help fight the disease.
Twenty saw their tumours shrink or disappear altogether, while nearly one in five (19%) experienced some improvement.
“We don’t see much activity from the immune system in prostate tumours, so many oncologists thought immunotherapy wouldn’t work for this cancer type,” study author Professor Johann de Bono, from The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, said.
“But our study shows a small proportion of men with end-stage cancer do respond”.
Prostate cancer affected 47,740 new men between 2014 and 2016 in the UK, Cancer Research UK statistics show.
In the US, 174,650 men are expected to be diagnosed by the end of the year, according to the American Cancer Society.
Survival rates are generally good, with around 84% still alive a decade or more after their diagnosis.
READ MORE: Proton therapy for prostate cancer: does the evidence support the hype?
Although the number of men whose tumours shrank or vanished was relatively small, others also benefited.
Some 166 of the participants had particularly advanced disease and high levels of PSA, a protein that can be a sign of prostate cancer. Pembrolizumab is said to have extended their lives by an average of around eight months.
Of these, nine also saw their disease disappear, either completely or partially, on scans.
And four were alive and well once the trial ended, despite having a very poor prognosis at the start. Dubbed “super responders”, this lasted at least 22 months.
“Our study has shown a small proportion of men with very advanced prostate cancer are super responders to immunotherapy and could live for at least two years and possibly considerably longer,” Professor de Bono said.
“Two of my own patients who have now been on the drug for more than two years”.
Among patients whose PSA levels were low but the disease was in their bones, pembrolizumab helped them live another 14 months.
The immunotherapy is thought to particularly benefit men with the protein PD-L1 in their tumours, with them surviving 9.5 months compared to 7.9 months for those with other forms of the disease.
Cancer cells may use the PD-L1 pathway to hide from the immune system. By blocking this pathway, pembrolizumab helps the immune system detect and fight malignant tumours.
However, testing for PD-L1 alone is not enough to gauge a patient’s pembrolizumab response, the UK scientists claim.
READ MORE: Metastatic Prostate Cancer: Symptoms, Medications and More
Pembrolizumab was also found to be “well tolerated”, with 60% experiencing side effects, of which 15% were “severe”.
The drug, which can attack healthy tissue, is known to cause colitis, hepatitis and kidney failure.
Tests are needed to identify those who could benefit from the drug, the scientists added.
Larger trials are investigating whether pembrolizumab could help those with “DNA repair gene mutations” on their tumours or whose cancer has spread to their bones.
This comes after a study released last week found the drug may be five times more effective than chemotherapy against head and neck cancer.
In the US, pembrolizumab is approved to treat a range of cancers that cannot be surgically removed or have progressed despite treatment. These include advanced melanoma, stomach or cervical cancer.
NHS England announced in June last year it will be routinely available for patients with lung cancers that have spread. It could already be dished out for patients with melanoma or Hodgkin lymphoma.


