The ultimate guide to travel vaccinations

Wherever your travels take you, whatever the purpose of your trip, finding out about likely health risks at your destination – and how to reduce them – is a vital part of ensuring a successful and enjoyable time away.
A specialist travel clinic is a good place to start, for a careful review of your past vaccination protection and any additional vaccines you may need. Some destinations require proof of vaccination against dangerous endemic diseases, such as yellow fever, on entry to the country, and some disease-prevention regimens begin far before the day of departure, so it’s important to be aware of sensible precautions as you look ahead to your trip.
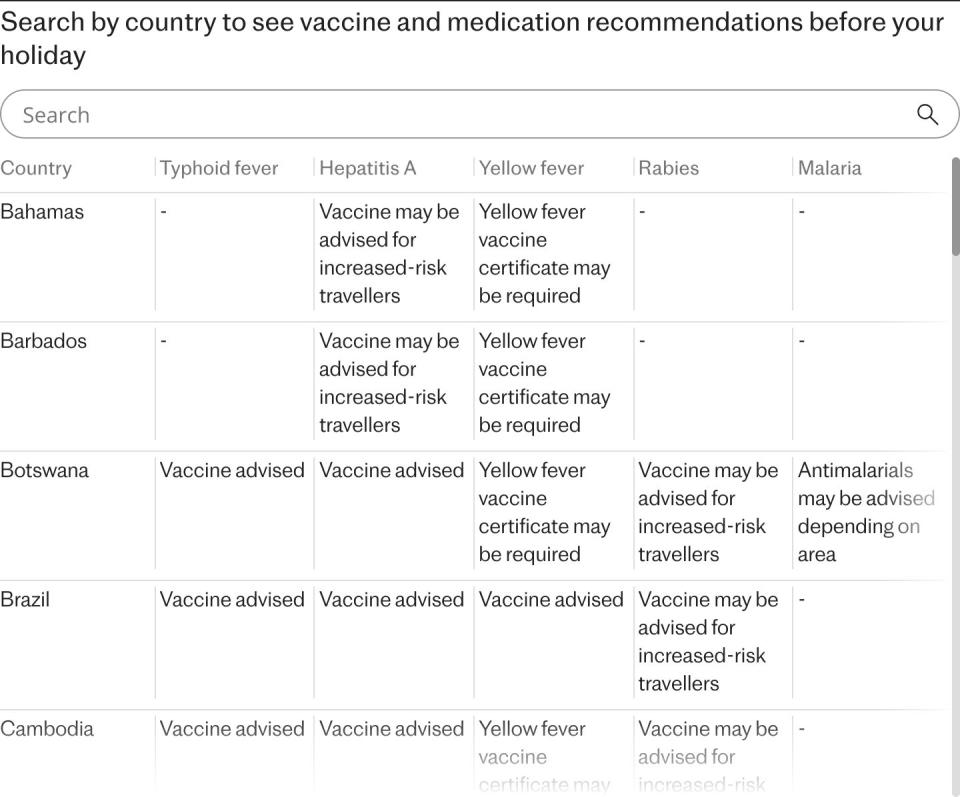
Here are the most common diseases travellers might encounter abroad, how and when to vaccinate against them, and how to mitigate risks of illness on holiday.
In this guide:
Typhoid
Risk areas: Africa, the Indian subcontinent, south and south-east Asia and South America
Method of inoculation: Vaccine (injection or oral medication) every three years
When to get vaccinated: At least one month before travel
What is typhoid?
Typhoid is caused by salmonella bacteria, with fever, diarrhoea (or sometimes constipation) and potentially serious complications. Drug resistance can make it difficult to treat.
What to know about the typhoid vaccine
It needs updating every three years. If you hate needles, an oral typhoid vaccine is available as an alternative.
Hepatitis A
Risk areas: Africa, Asia, the Middle East, and Central and South America
Method of inoculation: Injection
When to get it: Two weeks before travel
What is hepatitis A?
Hepatitis A is a viral infection of the liver – and complications such as liver failure increase with age. The good news: hepatitis A is now rare in travellers since vaccines became available in the 1990s.
What to know about the hepatitis A vaccine
Your first dose protects for a year; a second dose extends this to more than 20 years.
Yellow fever
Risk areas: Sub-Saharan Africa, South America, Central America and Trinidad in the Caribbean.
Method of inoculation: Injection
When to get it: More than 10 days before travel
What is yellow fever?
Yellow fever is a viral infection spread by mosquitoes in Africa and Latin America. Though named after the yellowing produced by liver failure and jaundice, the virus attacks every system of the body. It occurs in sudden, unpredictable outbreaks interspersed with inactivity.
What to know about the yellow fever vaccine
The vaccine is given only at officially authorised vaccinating centres. It contains live, weakened virus that may cause ill effects in older age groups or in people with various pre-existing medical conditions, so a careful risk assessment is essential. Yellow fever vaccination certificates are valid for life – but only become valid 10 days after vaccination. Some experts recommend booster doses at 10 years for those at high ongoing risk.
Expert tip: Countries with mosquitoes capable of spreading yellow fever often require travellers coming from yellow fever zones to show proof of vaccination as a condition of entry – to prevent spreading the disease – so check requirements carefully.
Rabies
Risk areas: Asia, Africa, and Central and South America
Method of inoculation: Three jabs for pre-travel vaccination
When to get it: At least eight weeks before travel
What is rabies?
Rabies is a fatal viral infection of the brain and nervous system. All bites, licks and scratches by dogs (or other mammals, including monkeys, cats and bats) must be treated as a potential rabies risk. Rabies occurs in most countries, and animal bites are among the most frequent reasons for travellers to need medical care abroad.
What to know about the rabies vaccine
Ideally, three doses of vaccines are needed, over three weeks. Pre-travel vaccination greatly simplifies the action needed if bitten while on holiday: cleansing the wound to prevent infection and promote healing, and booster vaccine doses as soon as possible.
Without prior vaccination, treatment is more complicated and more urgent: an injection of rabies immune globulin (RIG) – a product containing antibodies that neutralise rabies virus that is often unavailable in countries with the highest risk – into the area of the bite. This treatment is followed by an accelerated course of vaccine, which can throw your travel itinerary into chaos revolving around medical appointments.
Expert tip: Never handle animals while travelling. Street dogs are a particular hazard: they are not pets, can be territorial, and should not be approached. Docility can be a sign of rabies, and sick or injured animals should not be touched. And infamous “monkey temples” should be observed only from a distance.
Malaria
Risk areas: Parts of Africa and Asia, Central and South America, Dominican Republic and Haiti, parts of the Middle East, and some Pacific islands
Method of inoculation: Tablets or capsules
When to get it: Speak to a doctor four to six weeks before travel
What is malaria?
Malaria parasites are transmitted by Anopheles mosquitoes. Symptoms include fever, chills, aching muscles and joints, headache, abdominal pain, diarrhoea and jaundice – if untreated, can lead to reduced consciousness, coma and possibly death. Symptom onset may be delayed for weeks, when the connection to travel may be forgotten. (Read more about the rising cases of malaria in our guide to preventing the disease while abroad.)
What to know about antimalarial treatments
Antimalarial tablets or capsules, the most common being Malarone and doxycycline, are usually taken once a day before, during and after travel.
Expert tip: If you become unwell upon returning home, always tell your doctor you have been away so they can do appropriate tests for malaria.
Dengue fever
Risk areas: Parts of Africa and Asia, Central and South America, the Caribbean, the Pacific islands, and some southern areas of North America. (However, dengue’s geographic range is extending as warmer temperatures create more favourable conditions, with sporadic cases even in southern Europe.)
Method of inoculation: Vaccine injection (for high-risk travellers only)
When to get it: Speak to your doctor more than three months before travel if you are at high risk of illness
What is dengue?
Dengue is the world’s most common mosquito-borne viral infection. Also known as “break-bone fever”, symptoms include a rash, and pain in muscles, joints and behind the eyes. There are four different strains – infection with one strain only gives partial protection against future infection with a different strain. Subsequent infections can be more serious.
What to know about the dengue vaccine
A dengue vaccine has recently been licensed in the UK, given in two doses, three months apart; if this is impracticable, an initial dose provides 80 per cent protection. Some experts worry about the possibility of an increased risk of future severe dengue, and therefore recommend only vaccinating travellers with a previous dengue infection – so it’s best to speak to your GP or a travel health specialist about any concerns.
Expert tip: The best way to prevent dengue infection is to prevent mosquito bites.
How to protect yourself on your travels
We all want our travels to be relaxing and care-free: taking a proactive approach to health, prevention and your own safety is crucial to their success. Follow these tips to stay safe on holiday.
Bite prevention
Protecting yourself from insect bites is a good way to avoid several of the diseases detailed above – and also the nuisance of bites themselves. In fact, careful insect precautions can reduce numbers of bites by 90 per cent or more: used together, bite prevention measures, vaccines and anti-malarial medication are a powerful combination.
When outdoors at times when mosquitoes are biting, cover up and use insect repellents containing 50 per cent DEET on clothing and exposed skin (repellents containing picaridin are also effective). Clothing can be sprayed with permethrin, which is safe for humans but a contact killer for insects. When sitting outdoors, burn mosquito coils to keep mosquitoes away. Indoors, in screened or air-conditioned rooms, use spray insecticides combined with plug-in insect killers. At night, if mosquitoes can enter your accommodation, sleep under a bed net kitted with insecticide.
Food and water hygiene
There’s no polite way to say this: food, water and hands contaminated directly or indirectly with faeces spread diarrhoeal illnesses, viruses, parasites, bacteria and their toxins. The risk rises with hot temperatures and poor hygiene, and it can be especially difficult to avoid when off guard (on a recent trip to the United States, my pride was severely dented by a bout of Shigella dysentery, traced to an outbreak caused by contaminated guacamole – albeit rapidly tested for and treated).
Fresh, thoroughly cooked food, served hot is safest. Remember to wash your hands frequently, and use hand sanitisers or wipes. Buffets – especially in warm temperatures and where flies are present – are highly risky; choose freshly cooked food instead. Where hygiene is poor, avoid salads and raw food.
A tough but effective call for warm climates: avoid ice in drinks and stick to bottled water. And to be prepared for worst case scenarios, travel with a medical kit containing diarrhoea treatment, oral rehydration tablets and antibiotics.
Information to tell your doctor
The best way to ensure you’re protected ahead of any travels abroad is to speak to a doctor, sharing your upcoming itinerary and any high-risk activities planned – such as animal encounters or wilderness excursions. Your GP can also help identify any routine vaccinations needed, such as measles, diphtheria, whooping cough, tetanus, polio and more commonplace illnesses like Covid and flu.
Where to learn more
For more information visit Travel Health Pro and Fit For Travel.
Dr Richard Dawood is a specialist in Travel Medicine at the Fleet Street Clinic


