Superbug crisis threatens to kill 10 million per year by 2050. Scientists may have a solution
Cynthia Horton’s earaches are the stuff of nightmares.
“I can wake up from my sleep in horrible pain, like I’m having a root canal with no anesthesia,” she said. “When I sit up, my ear is often weeping with infection, even oozing blood.”
Already weakened by a lifelong battle with lupus, Horton’s immune system was devastated by rounds of radiation and chemotherapy after a 2003 surgery for a cancerous tumor in her ear.
Ear infections became the norm, usually eased by a round of antibiotics. But as the years passed, the bacteria in 61-year old Horton’s ear became resistant to antibiotics, often leaving her with little to no relief.
“These multi-drug-resistant superbugs can cause chronic infections in individuals for months to years to sometimes decades. It’s ridiculous just how virulent some of these bacteria get over time,” said Dwayne Roach, assistant professor of bacteriophages, infectious disease and immunology at San Diego State University.
Last year doctors offered to treat Horton’s infection with one of nature’s oldest predators — tiny tripod-looking viruses called phages designed to find, attack and gobble up bacteria.

The microscopic creatures have saved the lives of patients dying from superbug infections and are being used in clinical trials as a potential solution to the growing problem of antibiotic resistance. In the United States alone, more than 2.8 million antimicrobial-resistant infections occur each year.
Such infections are a “urgent global public health threat,” killing 5 million people worldwide, according to 2019 statistics from the US Centers for Disease Control and Prevention.
“It’s estimated that by 2050, 10 million people per year — that’s one person every three seconds — is going to be dying from a superbug infection,” said infectious disease epidemiologist Steffanie Strathdee, codirector of the first dedicated phage therapy center in North America, the Center for Innovative Phage Applications and Therapeutics, or IPATH, at UC San Diego School of Medicine.
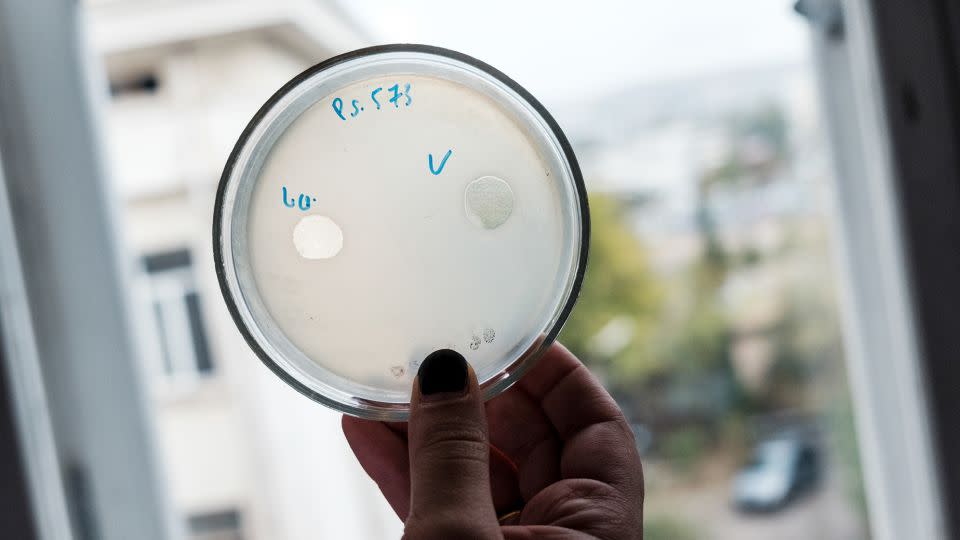
Eager for a different solution to her recurrent ear infections, Horton was game. Samples of her drug-resistant bacteria were shipped from her doctor’s office in Pennsylvania to UC San Diego’s IPATH with the hopes that phage hunters there could find a match. What scientists discovered next, however, was unexpected.
The bacteria cultured from Horton’s ear were a perfect match to a rare superbug found in certain brands of over-the-counter eye drops that were robbing people of their vision and lives.
Suddenly, the search for a solution to Horton’s problem took on new meaning. Would the bacteria from her ear help scientists find phages that would treat the eye infections as well?
Long-lasting and contagious
Severe cases of antibiotic-resistant eye infections began popping up in May 2022. By the following January, the CDC said at least 50 patients in 11 states had developed superbug infections after using preservative‐free artificial tears. By May 2023, the outbreak had spread to 18 states: Four people died, another four lost eyes, 14 suffered vision loss, and dozens more developed infections in other parts of the body.
“Only a fraction of patients actually had eye infections, which made the outbreak incredibly difficult to solve,” said epidemiologist Dr. Maroya Walters, who led the CDC’s artificial tears investigation.
“We saw people who were colonized by the organism develop urinary tract or respiratory tract infections months down the road, even though they were no longer using these drops,” Walters said. “One patient spread the infection to others in the health care facility.”
The culprit was a rare strain of drug-resistant Pseudomonas aeruginosa that had never been identified in the United States before the outbreak, the CDC said.
Horton had never used eye drops, yet the bacteria cultured from her ear were the same rare strain. Using those bacteria and other samples sent by the CDC, scientists at IPATH immediately went to work and identified more than a dozen phages that successfully attacked the deadly pathogen.
Scientists at the CDC were intrigued by the discovery, so much so that they mentioned the availability of the phage treatment for the superbug on the CDC website.
“It brought up this idea of when we have an outbreak that’s caused by bacteria with such limited treatment options, should we be thinking about these alternative therapies?” Walters said.
What is this little creature that can topple bacteria capable of withstanding all the drugs that modern science can muster? And more importantly, could phage treatment become a major player in the battle to end the superbug crisis?
The microscopic war inside us
Thanks to evolution, the gazillions of bacteria in the world today have a natural enemy: tiny viruses called bacteriophages genetically programmed for search-and-destroy missions. In this microscopic game of “The Terminator,” each set of phages is uniquely designed to find, attack and devour a specific type of pathogen.

“Each bacterial species, or even genotypes within it, can have a whole repertoire of phages that are attacking it, using a wide variety of methods to enter and debilitate the bacterial cell,” said Paul Turner, a professor of ecology and evolutionary biology at Yale University and microbiology faculty member at Yale School of Medicine in New Haven, Connecticut.
To counter the attack, bacteria employ various evasive maneuvers, such as shedding their outer skins to eliminate docking ports the phage use to enter, ravage and ultimately explode the pathogen into bits of bacterial goo.
That’s good news because the newly naked bacteria may lose their resistance to antibiotics, becoming once again vulnerable to elimination. The phage, however, is taken out of action, no longer able to fight.
To maximize success, specialists search for a variety of phages to tackle a particularly nasty superbug — at times creating a cocktail of microscopic warriors that can hopefully continue the attack when one is neutralized.
That’s what happened in 2016 to Strathdee’s husband, Tom Patterson, a retired professor of psychiatry at UC San Diego. Due to an infection with “Iraqibacter,” a drug-resistant bacterium found in the sands of Iraq, Patterson was in multi-organ failure and perilously close to death. In a race against time, Strathdee overcame incredible obstacles to find and deliver several cocktails of purified phages to Patterson’s doctors.
One of those cocktails contained a phage that “scared the bacteria so much that it dropped its outer capsule,” said Strathdee, an associate dean of global health sciences at UC San Diego and coauthor of “The Perfect Predator: A Scientist’s Race to Save Her Husband From a Deadly Superbug.”
“It was more afraid of the phage, if you will, than the antibiotic, and that allowed the antibiotic to work again. It was the one-two punch Tom needed,” Strathdee said. “Three days later, Tom lifted his head off the pillow out of a deep coma and kissed his daughter’s hand. It was just miraculous.”

Phage therapy 3.0
In labs around the country, phage scientists are taking research and discovery to the next level, or what Strathdee calls “phage 3.0.” Scientists in Turner’s Yale laboratory are busy mapping which phages and antibiotics are most symbiotic in the fight against a pathogen. Roach’s San Diego State lab is investigating the body’s immune response to phages while developing new phage purification techniques to prepare samples for intravenous use in patients.
Currently, clinical trials are underway to test the effectiveness of phages against intractable urinary tract infections, chronic constipation, joint infections, diabetic foot ulcers, tonsillitis and the persistent, reoccurring infections that occur in patients with cystic fibrosis. The chronic infections common in cystic fibrosis are typically due to various strains of drug-resistant Pseudomonas aeruginosa — the same pathogen responsible for Horton’s ear infection and the artificial tears outbreak.
A number of labs are developing libraries of phages, stockpiled with strains found in nature that are known to be effective against a particular pathogen. In Texas, a new facility is taking that a step further — speeding up evolution by creating phages in the lab.
“Rather than just sourcing new phages from the environment, we have a bioreactor that in real time creates billions upon billions of phages,” said Anthony Maresso, associate professor at Baylor College of Medicine in Houston.
“Most of those phages won’t be active against the drug-resistant bacteria, but at some point there will be a rare variant that has been trained, so to speak, to attack the resistant bacteria, and we’ll add that to our arsenal,” Maresso said. “It’s a next-generation approach on phage libraries.”
Maresso’s lab published a study last year on the treatment of 12 patients with phages customized to each patient’s unique bacterial profile. It was a qualified success: The antibiotic-resistant bacteria in five patients were eradicated, while several more patients showed improvements.
“There’s a lot of approaches right now that are happening in parallel,” Roach said. “Do we engineer phages? Do we make a phage cocktail, and then how big is the cocktail? Is it two phages or 12 phages? Should phages be inhaled, applied topically or injected intravenously? There’s a lot of work underway on exactly how to best do this.”
To date, genetic manipulation of phages has been difficult due the streamlined nature of the creature: “Normal phages are optimized by evolution to be lean, mean, killing machines. There’s very little room in there for us to get in and change things,” said Elizabeth Villa, a professor of molecular biology at UC San Diego who studies a new form of phage called “jumbo” phages.
“Jumbo phages have very large genomes and come close to having a nucleus that encapsulates the genetic material, which protects them from some of the mechanisms bacteria use against phages to deactivate them,” said Dr. Robert “Chip” Schooley, a leading infectious disease specialist at UC San Diego who is codirector of IPATH.
“That also gives them room to be engineered to become more potent, so they’re very promising phages to be used therapeutically,” Schooley said.
Genetically engineering phages would allow scientists to target each person’s unique mix of antibiotic-resistant pathogens instead of searching sewage, bogs, ponds, the bilge of boats and other prime breeding grounds for bacteria to find just the right phage for the job.
Along with phage libraries, genetic engineering is also a key to churning out phages in mass, to distribute on a wider scale. In Russia and the country of Georgia, where phage therapy has been used for decades, patients can buy phage cocktails off the shelf in pharmacies.
All this work has caught the attention of the CDC. In addition to using a phage cocktail to treat a superbug outbreak in real time, phages could also help fight a broader issue — the recolonization of the infected person with the same superbug, the CDC’s Walters said.
“The issue is that when patients have infections with these drug-resistant bacteria, they can still carry that organism in or on their bodies even after treatment,” Walters said. “They don’t show any signs or symptoms of illness, but they can get infections again, and they can also transmit the bacteria to other people.”
However, if phages could be used to “decolonize” a bacterial population inside a high-risk person, “patients could really decrease the likelihood of developing an infection and spreading to others, which is a big part of the problem,” Walters said.
“We were thinking about trying to develop a curated phage collection that would be active against a large number of certain resistant organisms,” she added. “Pseudomonas is a good place to start — there are more than 140 different species. But there are many other organisms that threaten us that we also need to tackle.”
For more CNN news and newsletters create an account at CNN.com


