What is vitiligo? The rare skin condition explained

A condition that causes the skin to lose pigmentation, vitiligo affects around one per cent of the UK population.
The long-term disorder, in which white patches of skin appear on different parts of the body, is caused by a lack of pigment called melanin and is thought to be an autoimmune condition.
In recent years, vitiligo has become more widely recognised thanks to celebrities like supermodel Winnie Harlow discussing and breaking barriers associated with the condition.
The 24-year-old gained prominence as a contestant on US television series America’s Next Top Model in 2014 and has since appeared on the runway for some of the fashion industry’s biggest designers including Victoria’s Secret and Marc Jacobs.
From what causes it to the different types and treatment options, here’s everything you need to know about vitiligo:
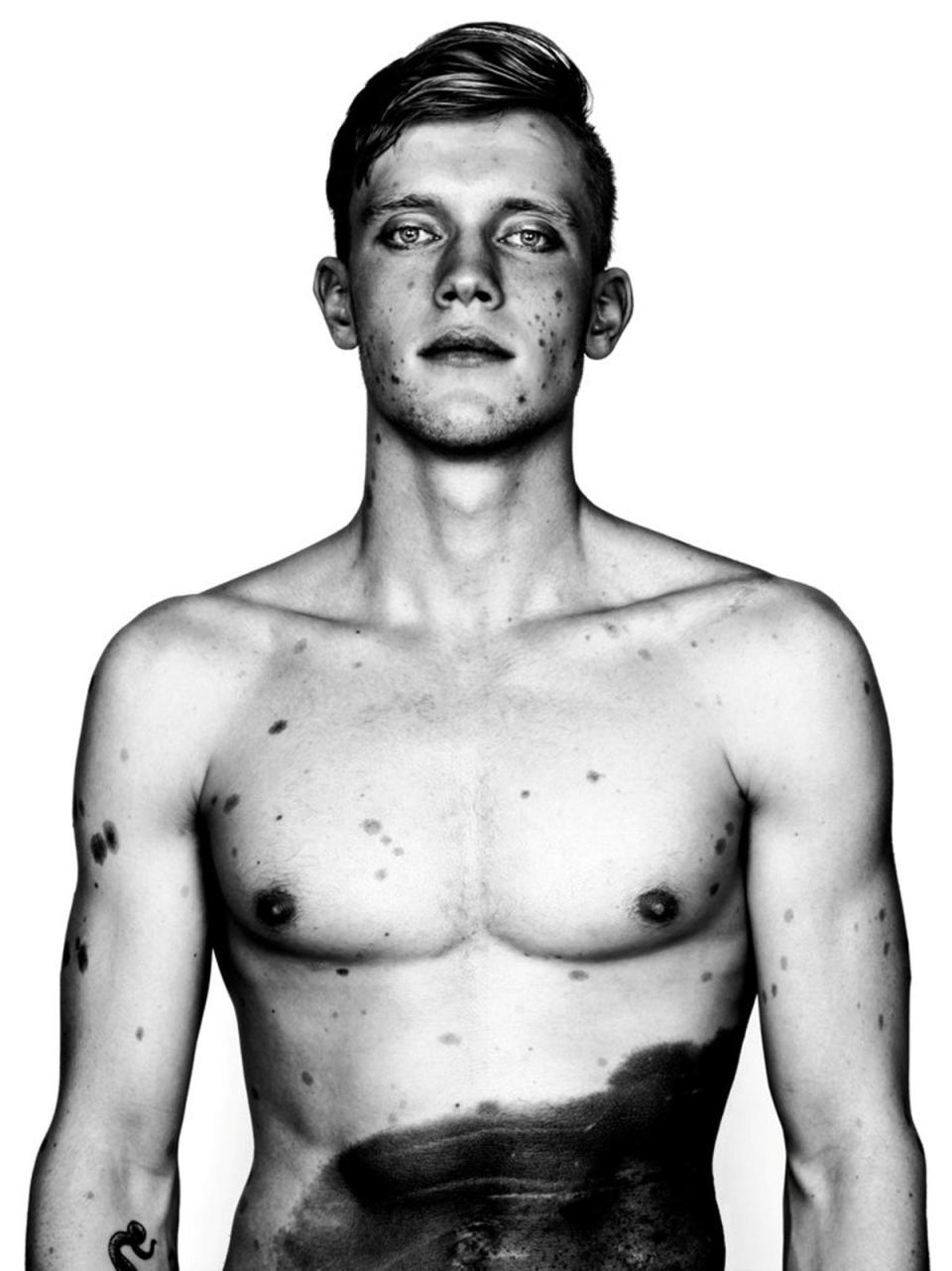
Congenital skin conditions presented in empowering photography exhibit









What is vitiligo?
Vitiligo is a long-term condition where pale patches develop on the skin, the NHS states.
Typically, vitiligo can affect any area of the skin, but it most commonly occurs on the face, neck and hands, and in skin creases.
According to the British Skin Foundation, vitiligo can start at any age after birth but in more than half of people affected it does so before 20 years of age.
The extent of the condition is unpredictable, varying from single small patches to total loss of skin colour. In most people, it tends to change slowly, with periods of stability often lasting several years.
There are two types of vitiligo: segmental and non-segmental.
Non-segmental vitiligo is the most common type, affecting around nine out of 10 people with the condition. The symptoms often appear on both sides of your body as symmetrical white patches.
With segmental vitiligo, also known as unilateral or localised vitiligo, the white patches only affect one area of your body.
What causes vitiligo?
Non-segmental vitiligo is also thought to be an autoimmune condition, the NHS states.
This means that a person’s immune system destroys the melanocyte skin cells that make melanin and give your skin its colour.
Meanwhile, segmental vitiligo is thought to be caused by chemicals released from the nerve endings in your skin. These chemicals are poisonous to the melanocyte skin cells.
The British Skin Foundation also states that vitiligo can be hereditary.
“Vitiligo has a genetic basis, although less than half of those with vitiligo know of someone in their family who also has it. If you have vitiligo, it does not necessarily follow that your children will develop it.”
The NHS states that it is possible for vitiligo to be triggered by particular events such as childbirth, skin damage and exposure to certain chemicals.
Can vitiligo be treated?
There is no cure for vitiligo and while treatment can be helpful in restoring the colour, it cannot prevent its spread or recurrence.
Typically, treatment options are based on improving the appearance of the skin using phototherapy – treatment with light – medication and camouflage creams.
The British Skin Foundation states that often no treatment may be required but that options can include:
Sunscreens. Areas of vitiligo will burn easily in the sun. The use of a sunscreen with a high sun protection factor (SPF) of 30 or higher to all exposed areas helps to protect skin affected by vitiligo, and also, when applied more widely, reduces the contrast between the areas of vitiligo and the surrounding normal skin.
Topical corticosteroids. The application of a potent or very potent corticosteroid anti-inflammatory cream or ointment to areas of vitiligo may restore some pigment. Side effects, such as thinning of the skin and stretch marks, are a risk with continued use. Short courses of oral steroids can sometimes be considered but may be associated with side effects such as weight gain, skin thinning, mood changes and cataracts.
Other topical preparations. Other types of anti-inflammatory creams and ointments, such as calcineurin inhibitors and vitamin D analogues, may also restore pigment in some patients. These topical treatments will help avoid the corticosteroid side effect of skin thinning.
Phototherapy. This involves exposing affected skin to artificial ultraviolet light. Phototherapy may be helpful in a proportion of patients with vitiligo. However, treatment often needs to be prolonged (lasting at least several months). Full repigmentation is unusual and depigmentation after phototherapy can occur. Areas such as the fingertips and the skin around the lips are less likely to improve (see Patient Information Leaflet on Phototherapy). Phototherapy may also be used in combination with topical or oral corticosteroid treatments.
Surgical treatment. This process involves transplanting small areas of normal skin into areas of stable vitiligo. This method of treatment is still being developed and is not yet in general use.
Laser treatment. Some areas of vitiligo have improved from treatment with a laser called the Excimer laser. This treatment appears to work best on vitiligo that has not changed for a long time and affects relatively small areas of skin. Laser treatment can sometimes be used in combination with topical treatments.
Removing the remaining pigment. If vitiligo has spread very widely (more than 50% of the body) or involves large areas of the face or hands, it may in exceptional circumstances be reasonable to consider removing the small amounts of pigmented areas of skin using a bleaching chemical such as hydroquinone. The emotional, social and medical implications must be carefully discussed before this treatment is used and it should only be undertaken with specialist supervision.
Psychological treatments.Professional help with developing coping mechanisms may be helpful for some people with vitiligo or their carers e.g. parents.
Skin camouflage. Advice from experts about skin camouflage is now widely available. There are good quality camouflage products in a range of colours that are water resistant and less likely to rub off. Your GP or dermatologist can advise or refer you to a camouflage service for this. Careful use of fake suntans can be effective to make areas of vitiligo less noticeable.
For more information or support you can contact the Vitiligo Society – a national charity whose main aim is to support people with vitiligo – on 0800 018 2631.

















