What is super-gonorrhoea, what are the symptoms and how can it be treated?
It’s been reported that two women who contracted a rare form of super-gonorrhoea did so while having unprotected sex in Ibiza.
According to a new study, published in medical journal Eurosurveillance, one of the women first showed symptoms of the condition when she visited a sexual health clinic in October 2018.
A month later, the second woman, who was part of the “same sexual network” as the first, also discovered she’d contracted the STI after visiting a health clinic.
Super-gonorrhoea is far more rare than gonorrhoea, which is the second most common bacterial sexually transmitted infection in the country.
So what are the symptoms of super-gonorrhoea, how can it be treated and how can it be prevented?
Here’s everything you need to know:
What is it?
Gonorrhoea is a sexually transmitted disease otherwise known as “the clap”.
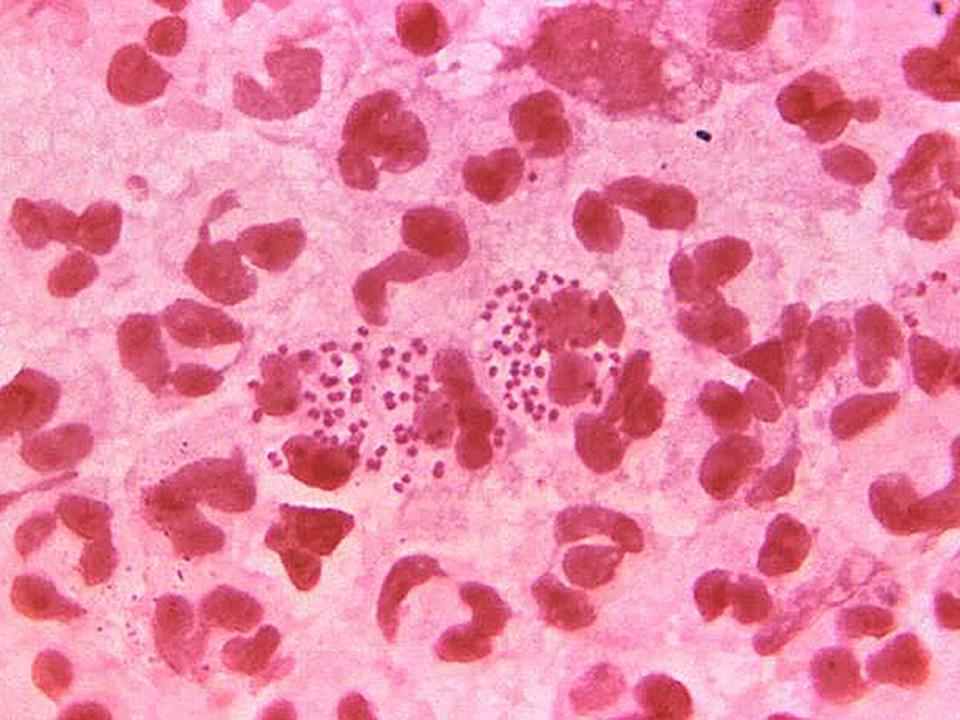
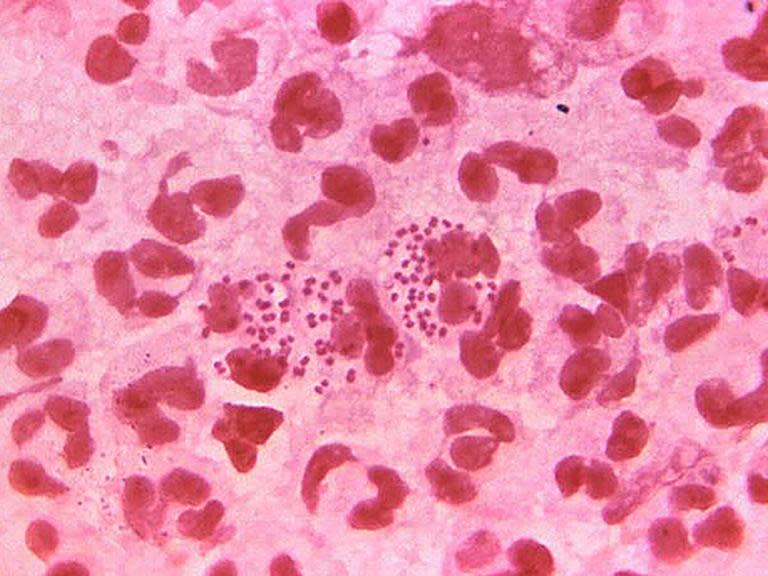
It’s caused by bacteria called Neisseria gonorrhoeae, also called gonococcus, which is usually found in penis discharge and vaginal fluid.
It can be spread through vaginal, oral or anal sex, or by fingers if they’ve been in contact with the disease.
Super-gonorrhoea is a more severe strain of gonorrhoea, as medical director of Terrence Higgins Trust Michael Brady explains.
“So called ‘super gonorrhoea’ refers to strains of the infection that have become resistant to the antibiotics we usually prescribe to treat gonorrhoea; which means an alternative treatment needs to be found,” he tells The Independent.
While using a condom doesn’t completely eliminate the risk of spreading the disease, the risk can be “substantially reduced“ if condoms are used consistently and responsibly, says Dr Nick Phin, deputy director of the National Infection Service at Public Health England.
What are the symptoms?
Symptoms of gonorrhoea in men may appear within 10 days. However, often women affected by the disease experience no symptoms at all.
Men who’ve been infected with gonorrhoea may experience a yellow, white or green discharge from the penis, a burning feeling during urination and swelling around the foreskin, the Terrence Higgins Trust states.
For women, they may notice a change in their vaginal discharge, a burning feeling during urination and excessive bleeding in between their periods.
If an individual has been infected with gonorrhoea in their throat or rectum, they may not have any symptoms.
However, gonorrhoea in the rectum can lead to discharge or feelings of discomfort.
How can it be treated?
When getting tested for gonorrhoea, a swab may be used to take a sample from a woman’s vagina or from a man’s penis. Alternatively, men be asked to provide a urine sample instead.
Brady recommends getting tested for sexually transmitted diseases regularly if you’re having unprotected sex or sleeping with more than one partner.
Gonorrhoea can typically be treated with a course of antibiotics. However, super-gonorrhoea is a strain of gonorrhoea that’s far more difficult to treat.
According to the NHS, a diagnosis of gonorrhoea shouldn’t lead to any long-term complications as long as it’s treated early.
If a case of gonorrhoea isn’t treated appropriately, then it can spread to other parts of your body and lead to other more serious health complications.
Treatment for the disease usually involves having an antibiotic injection and an antibiotic tablet, with symptoms expected to dissipate within a few days.
The two antibiotics used to treat gonorrhoea are azithromycin and ceftriaxone.
While super-gonorrhoea is resistant to azithromycin, it isn’t resistant to ceftriaxone, the Terrence Higgins Trust states.
However, in the recent cases of the two women who contracted super-gonorrhoea, they were resistant to both the drugs, despite being successfully treated by doctors.
“Antibiotic resistance is a growing problem both within sexual health and in other areas of medicine,” says Brady.
How can it be prevented?
In order to prevent the spread of gonorrhoea during sex, it’s important to use contraception such as condoms or Femidoms.
“Condoms remain the best way of protecting yourself against gonorrhoea and other STIs,” Brady advises.
“If you’ve struggled with condom use in the past, I would advise trying out the range of different shapes and sizes available to find one that works for you and your partner.”
Other forms of contraception, such as the contraceptive pill, don’t provide protection against gonorrhoea, the Terrence Higgins Trust outlines.
The charity also suggests using condoms or dental dams during oral sex to reduce your risk of contracting the disease.
If a pregnant woman has been diagnosed with gonorrhoea, it’s possible for the disease to be spread to her baby during childbirth, which can lead to the baby becoming infected with conjunctivitis.
The mother can prevent this by taking a course of antibiotics during pregnancy or while she’s breastfeeding.