One in four adults in England prescribed potentially addictive drugs last year
Almost 12 million adults in England were prescribed potentially addictive drugs such as sleeping pills and painkillers last year, with half taking them long-term, a new report says.
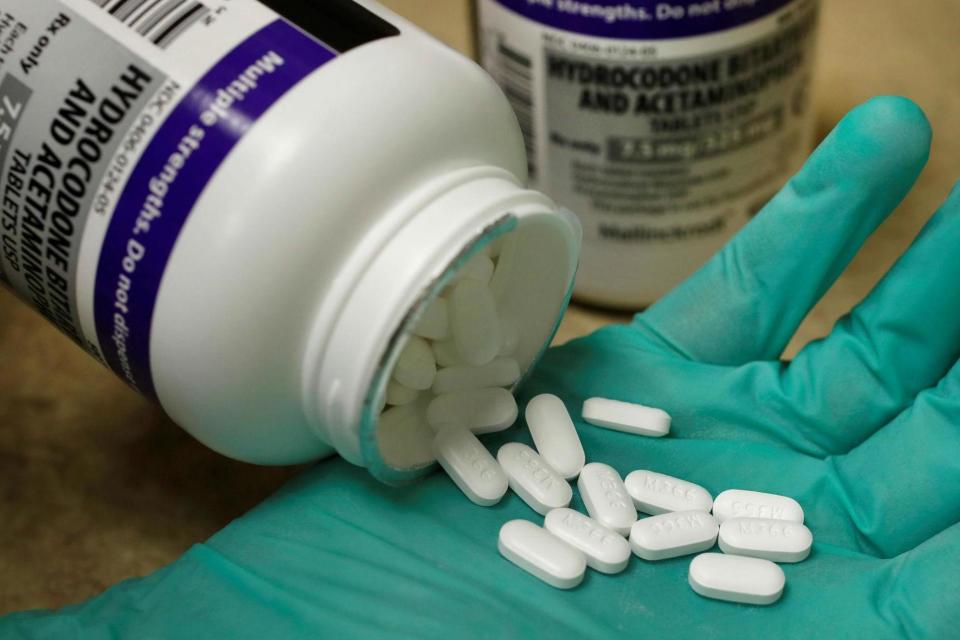
A review of five classes of medicines - including anti-anxiety drugs, anti-depressants and opioid painkillers - found some patients struggle to come off them, suffering suicidal thoughts and anxiety as a result.
Public Health England (PHE), which led the government-ordered review, said a helpline must be set up to help the millions of people who may be dependent on the drugs.
Since at least a decade ago, more people are being prescribed potentially addictive medicines and for longer periods of time, it said.
PHE looked at benzodiazepines, such as diazepam, which are commonly prescribed for anxiety and insomnia; Z drugs, gabapentinoids and opioid pain medications for non-cancer pain and anti-depressants.
It found one in four adults in England had been prescribed one of these drugs in the year up to the end of March 2018, with half of these having had a continuous prescription for at least the previous 12 months.
In one year, 17 per cent of the adult population were given anti-depressants, 13 per cent were given opioids, 3 per cent gabapentinoids, 3 per cent benzodiazepines and 2 per cent were given Z drugs.
Up to a third of people had been on the drugs for at least three years, including 930,000 people on anti-depressants, 540,000 on opioids and 160,000 on gabapentinoids.
Experts said opioids are known to be ineffective for most people over the long-term (more than three months), while benzodiazepines are not recommended for use for longer than 28 days.
PHE was unable to put an exact figure on how many people are addicted to the drugs long-term or who suffer problems when trying to come off them.
But it said patients must be warned via a national helpline and website about common side-effects of the drugs, advice on withdrawing from the medicines and what to expect, and advice on coping strategies.
It urged the public not to stop taking their drugs in light of the review but to speak to their GP if they had concerns.
The review made a series of other recommendations including more training for doctors, giving medics better access to data, including on prescribing rates in their area, and updating guidance on dependency and withdrawal problems.
It said doctors must also look to other therapies for their patients, such as cognitive behavioural therapy, or “social prescribing” of activities that might help, such as joining clubs or choirs.
Professor Paul Cosford, emeritus medical director at PHE, said some of the drugs, such as anti-depressants, do need to be taken in the long-term to realise their full effect but admitted he was “surprised” by the number of people on the drugs.
He said the review found that while most prescriptions were short-term, “significant numbers [of people] have been taking these medicines for a long time”.
He added: “We are not trying to stigmatise either these drugs or the people who take these drugs.
“When people are started on the drugs, it's in line with clinical guidance.
“What you see is that a proportion of those people then find it very difficult to withdraw from the drugs and end up on a long-term prescription.
“That proportion gradually builds because it accumulates over the years and that's the group we are particularly concerned about.”
The review found prescriptions for anti-depressants rose 10 per cent between 2016 and 2018, while prescriptions for gabapentinoids increased by 20 per cent.
However, prescriptions for opioids fell 3 per cent across the same period, Z drugs by 6 per cent and benzodiazepines by 8 per cent.
http://players.brightcove.net/624246174001/default_default/index.html?videoId=5837728067001
Support free-thinking journalism and subscribe to Independent Minds
The report found that, in March 2018, 513,000 people were taking both anti-depressants and opioids. Thousands more were taking a combination of three or more drugs.
Benzodiazepines and Z drugs can create long-term dependency and a risk of “rebound symptoms” when they are stopped, such as increased anxiety and sleep problems.
People coming off anti-depressants can also experience varying symptoms over the short-term including insomnia, nausea and flu-like symptoms.
Meanwhile, opioids are addictive while offering little long-term benefit.
Keith Ridge, chief pharmaceutical officer at NHS England, said the medicines could make a “big difference to people’s quality of life and for some their long-term use is clinically necessary”.
He added: “But for many patients they may not be the best option, with talking therapies and social prescribing often more appropriate.”
Press Association
Read more
Drug firm blamed for fueling opioid crisis 'offers up to $12bn'
Johnson & Johnson must pay $572m over opioid epidemic
Tate galleries shun Sackler family money over opioid crisis

