'My Epilepsy Was Misdiagnosed as Migraine & Anxiety for Years'
Affecting around one in 100 people in the UK, this complicated neurological condition is more than an aversion to flashing lights. To mark National Epilepsy Week this year, Anna Roberts - a 36-year-old journalist from London - explains the toll it takes on her mind...
There’s a Joy Division song about epilepsy called She’s Lost Control. ‘And seized up on the floor, I thought she’d died; she said, I’ve lost control again,’ it goes. Lead singer Ian Curtis, who took his own life in 1980, famously suffered from epilepsy and struggled with its mental health impact. Having lived with the condition for more than two decades, I’ve felt first-hand the repercussions it can have on your mind. At my best, I’m fine. At my worst, I can’t do anything.
All epilepsy is caused by misfiring electrical signals in the brain, but it’s their location that affects symptoms. Most epilepsy starts in the frontal and temporal lobes, but mine starts in the occipital lobe, the brain’s vision centre. Ahead of a seizure, I see sharp prisms of coloured light begin to form and, within minutes, they’ve clouded everything, while I feel a sickening sense of fear and confusion build.

I was 13 when I had my first seizure at a school netball match. To my – and my parents’ – distress, doctors didn’t know what was wrong. I struggled to articulate what was going on in my mind and body, instead getting upset and frustrated. The word ‘epilepsy’ never came up, and without a diagnosis – or the correct medicine – the seizures kept happening, with doctors attributing them to anxiety, migraines and hypochondria.
For the next 13 years, every time I left the house, the lingering fear that I could collapse and have a fit was omnipresent. But, determined that this glitch in my system wouldn’t dampen my ambition, I moved from Lincoln to Leeds to study English at university (where
I had just one fit), and did a master’s in journalism (during which I had two). They accelerated in number when I got my first job as a writer on a local paper, and then, when I began working shifts on a national newspaper in London, I collapsed three times on my first day and left in an ambulance. I was heartbroken to have lost control in a room filled with people I wanted to like and respect me.
Over the next few years, while I worked shifts at various newspapers, I fell unconscious in court, outside a police station, in the office, in the woods and in a branch of Tesco. Some people were supportive; others were scared – I was just furious and fearful that my career might be wrenched away from me. And so I returned to my doctor. Again, epilepsy was never mentioned; instead, my GP prescribed a medication used to treat migraines.
It just so happened that the primary function of that medication was to treat epilepsy, and so it worked. Over the next nine years, I didn’t lose consciousness once. With my medication, I was able to work, go out and form relationships like any other woman in her late twenties. The fear of collapse was there in my mind, but it faded into obscurity as each year passed, until it felt like a footnote in my past, rather than a shame-inducing headline in my present.
But then, in January 2019, I woke in the middle of the night unable to stop shaking. And after that fit, they continued. My vision deteriorated to such an extent that there were days where I couldn’t get out of bed – every time I opened my eyes, all I could see were those prisms of light. The shame and frustration returned with a vengeance. ‘You have occipital lobe epilepsy,’ the neurologist at Guy’s and St Thomas’ Hospital told me when I described my symptoms on our first meeting, after my GP had finally referred me to a specialist. It’s a rare form of epilepsy and difficult to diagnose, often mistaken for migraines. An EEG [a test detecting electrical activity in the brain] scan confirmed the diagnosis.
They weren’t clear on why symptoms soothed by my medication suddenly and unexpectedly worsened, but suggested stress might be a factor and that I needed to try some different formulations. One of the medications I tried worsened the seizures, which were horrific and left me spending my 35th birthday curled up in my bed; another made me so anxious I had daily panic attacks. One damaged my dwindling self-esteem further, leaving me with acne for the first time, while another gave me vertigo that left me bed-bound for a fortnight.
The episodes and subsequent anxiety – about when a fit would strike and all the things I was missing out on as I spent a year indoors – sent shockwaves through my life. By this point, I was working in my first full-time staff role at a national newspaper in London. My bosses gave me time off to recover – I was signed off for five months in April 2019 – plus access to a counsellor and company doctor, which helped. But it was around the same time that my relationship with my live-in partner ended. This only served to amplify the cold creep of anxiety and sense of loss over the life I felt I should have been living. Although, with the benefit of hindsight, it certainly made riding out a national lockdown the following year more bearable.
Right now, I’m doing pretty good: back working five days a week and taking a cocktail of medications daily that appear to be working. I’m well enough to feel excited about a summer enjoying unlocked pub gardens and day trips with friends. My anxiety is humming at a lower frequency, too. Above all, I’m slowly beginning to accept that, while I can do things to reduce my chances of having an episode, I don’t need to feel shame if I do, again, lose control.
Epilepsy and mental health: The expert view
Richard Selway is a consultant neurosurgeon specialising in epilepsy. He works at the London Neurosurgery Partnership at The Harley Street Clinic, part of HCA Healthcare UK
What is epilepsy?
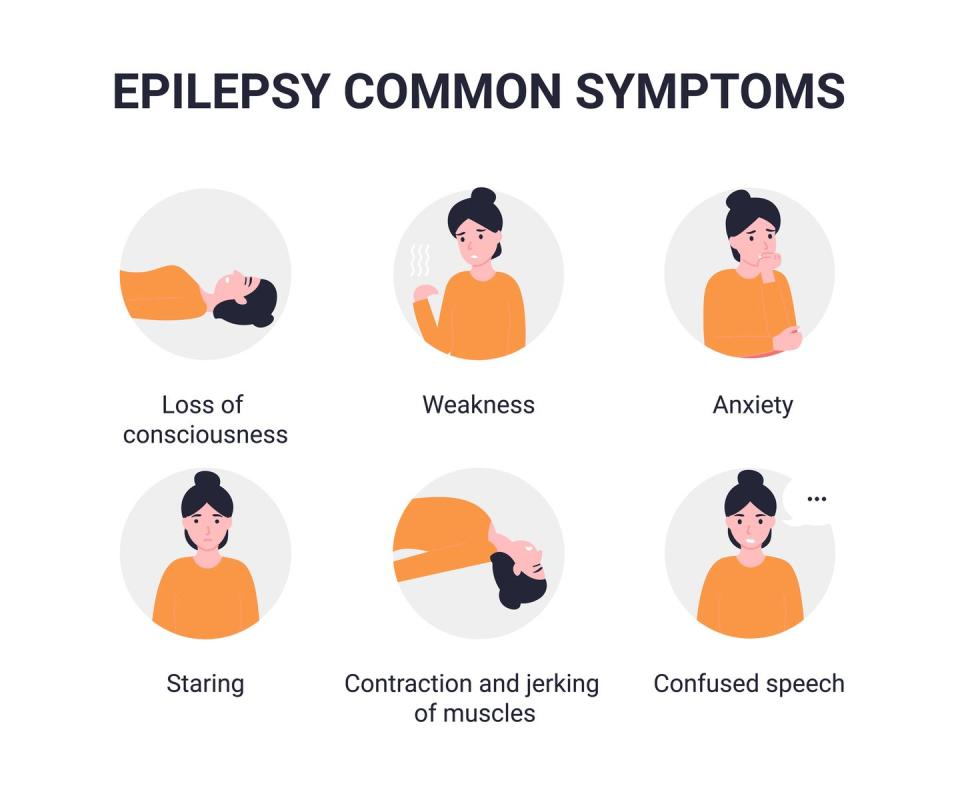
Epilepsy is the tendency to have repeated seizures, which affects about one in 100 people, so you probably know at least one person with the condition. A seizure is an electrical disturbance in the brain – a ‘short circuit’ – that causes that area to misfire. What seizures look or feel like will be determined by which part of the brain is involved. If a seizure starts in an area dealing with speech, then the sufferer may be unable to speak for a minute or two; in Anna’s case, it affects the visual areas, so vision is disturbed. If the seizure spreads right across the brain, it will cause a generalised tonic-clonic seizure, also known as a grand mal attack, characterised by a loss of consciousness and muscle contractions.
What impact can epilepsy have on your mental health?
A seizure can trigger anxiety by affecting parts of the brain involved in the fear response. However, the unpredictability of when an attack might occur is often a major cause of anxiety and can have a seriously limiting impact on sufferers. This can lead to lower life satisfaction and even depression. Harvard psychiatrists have estimated that as many as a third of people with epilepsy suffer from periodic depression and that epilepsy sufferers are four to seven times more likely to suffer with depression than the average person.
How can you help an epilepsy sufferer in your life?
If you see someone who’s collapsed, with their limbs shaking, cushion their head
and move any furniture away from them to avoid injury. If in doubt, or if the seizure continues for more than five minutes (the vast majority will stop after the first minute or two), you should call 999. Don’t put anything in their mouth or try to restrain them during the attack, but do roll them into the recovery position if they’re unconscious afterwards. But it’s not just about the actual attack – given the shame sufferers can experience, which can lead to developing mental health conditions, it’s important to reinforce that the condition doesn’t make them any less valuable as a person.
For more information on epilepsy or for support with managing symptoms, go to epilepsysociety.org.uk
Cut through the noise and get practical, expert advice, home workouts, easy nutrition and more direct to your inbox. Sign up to the WOMEN'S HEALTH NEWSLETTER.
You Might Also Like


