EastEnders' PrEP Storyline Is Crucial For The HIV+ Community – It Needs Normalising

A doctor tells Zack that he would advise his partner to start PrEP, a drug that prevents HIV.
In 1991, EastEnders’ Mark Fowler became the first mainstream British TV character to be diagnosed with HIV – now, more than three decades later, EastEnders’ current HIV-positive storyline shows how the realities of HIV have changed since the height of the AIDS epidemic.
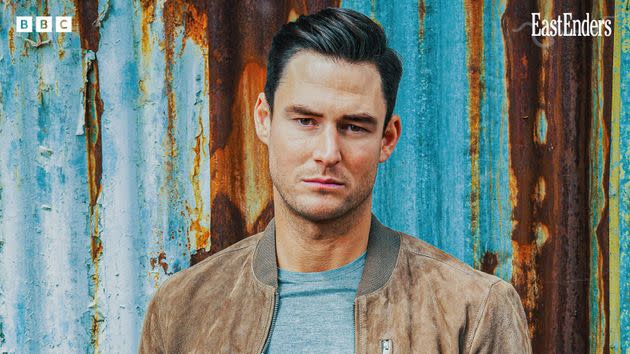
Zack Hudson (James Farrar) was diagnosed with HIV in a January episode of the show and for many viewers, Zack’s experiences will be their first exposure to modern HIV treatment. The BBC is working closely with Terrence Higgins Trust, the UK’s leading HIV and sexual health charity, to ensure the storyline is medically accurate.
One of the biggest changes since Mark’s storyline in the 1990s is the advancement of HIV treatment and prevention. In one of the soap’s recent episodes, a doctor tells Zack that he would advise his partner to start PrEP, a drug that prevents HIV.
So what is PrEP?
Pre-Exposure Prophylaxis (PrEP) is taken by people who are HIV-negative before and after sex, and reduces their risk of getting HIV. PrEP tablets contain two anti-antiretroviral medications – the same drugs used to treat people with HIV. Studies show PrEP is 99% effective in preventing HIV transmission when taken correctly.
Nowadays, PrEP is available for free on the NHS but, when PrEP was first approved by the US FDA in 2012, people started buying it from overseas because it wasn’t available on the NHS.
A key campaigner in the battle for free PrEP in England was Greg Owen, who works for Terrence Higgins Trust. Before the drug was made available for free via the NHS, Owen was doing sex work and working in a bar while sleeping on a friend’s sofa: he wasn’t able to afford the £150 it cost to buy three months’ worth of PrEP.
PrEP was finally made available to 10,000 people in England as part of a trial starting in September 2017, later expanding to 26,000. In October 2020, uncapped access was rolled out.
Owen says that free PrEP is crucial, as it’s often those who most need it most who can least afford it. However, because PrEP was initially only available if you could afford it, there’s still a misconception that you must pay for it.
Breaking HIV stereotypes
In Eastenders, Zack is a straight cis man, so his storyline combats another major misconception about HIV: the idea that the virus is only a concern for gay and bisexual men.
Terrence Higgins Trust reports that heterosexual people are far more likely to be diagnosed with HIV late, likely due to their belief that they’re not at risk of HIV.
63% of heterosexual men diagnosed in 2021 were at a late stage, meaning they’ve lived with HIV for at least three to five years and been unaware of it, at which point the virus has already started to damage their immune systems.
Currently, PrEP is only available through sexual health clinics in the UK. Regular STI testing is routine for many in the LGBTQ+ community, but many people still feel stigma and shame around visiting a sexual health clinic.
A report by the All Party Parliamentary Group on Sexual and Reproductive Health found that straight, cis women in particular prefer to access contraception and sexual health information through their GP.
This impacts their access to PrEP, which is concerning when women make up almost a third of the people in the UK who are HIV positive. A large proportion of those women are Black African women, who, Owen explains, are also the demographic who are least likely to be offered an HIV test.

There are two pills approved for use as PrEP: Truvada® and Descovy®.
Owen thinks it’s important to expand who can prescribe PrEP, and upskill GPs and community pharmacists to be able to serve the needs of patients who are uncomfortable or unable to visit sexual health clinics.
We need to keep talking about PrEP
Zack’s storyline will also help combat the lack of awareness of PrEP. Dr Will Nutland, a public health doctor and co-founder of PrEPster, says that this is an issue even within the LGBTQ+ community, especially among younger people.
After a decade of intense PrEP activism, the drug has somewhat fallen off the radar because we’re no longer fighting for it to be made available.
For those with multiple marginalised identities, PrEP is harder to access. Many sexual health clinics require you to call and book an appointment. Dr Nutland recalls sitting in his own clinic a few years ago and watching a Spanish-speaking patient come in and try to make a PrEP appointment: “In the end, the receptionist was so exacerbated with her inability to understand him – although she painted it as his inability to articulate to her – that she told him to leave the clinic.”
The most effective way to reach the people who would never set foot in a sexual health clinic because they’re worried about transphobia, homophobia or racism is by sending people from those communities to those communities.
This outreach work isn’t sexy or headline-grabbing; Dr Nutland explains that it’s underfunded, costly, and time-consuming. “You might go out and do an outreach shift and end up only speaking to three people, but those three people might well start PrEP. And those three people might be the people who most need to start PrEP today.”
If Zack’s partner, Whitney (Shona McGarty), does start PrEP, it will demonstrate that the drug is for people of all genders who are at risk of HIV. This is vital, as research conducted in 2022 by PrEPster and Terrence Higgins Trust, along with other organisations, found that no local authority in England had more than five women accessing PrEP. Owen thinks it’s important to position PrEP alongside other forms of contraception as part of a wider package for managing our sexual and reproductive health.
Zack is diagnosed with HIV after sharing needles through steroid use
EastEnders can reach people in a way that a health campaign or leaflet never would, and let them know that PrEP is a safe and well-tolerated medication. You can take PrEP if you’re trying to conceive, pregnant, or breastfeeding. It doesn’t interfere with hormonal contraception or trans people’s hormone replacement therapy. PrEP is safe to take with alcohol and viagra.
What EastEnders can’t – and shouldn’t have to – do is fix the issue that there simply isn’t enough funding going into sexual health services.
In parts of the UK, people are waiting up to 12 weeks to start PrEP – with some people testing positive for HIV while on that waiting list. Unable to access it through the NHS, some people reverted to buying PrEP online or borrowing the drug from friends.
Dr Nutland says: “Without an immediate reversal of these trends, and proper investment in sexual health, we can forget claims to be the first country to hit UNAID’s HIV targets by 2030.”
Zack’s storyline will highlight just how much progress has been made since EastEnder’s first HIV-positive character. Unlike Mark, current HIV treatments mean that Zack can have a child without any risk of passing on HIV to them. He will have the same life expectancy as someone who is HIV-negative.
Owen says it’s important that this information is being shared with such a wide audience: “With issues that affect minority communities and are heavily stigmatised, the antidote is the majority of people educating themselves.”
There isn’t a cure for HIV, but there is one for the stigma about the virus – the representation of people who are living long and healthy lives. Even today, that representation is incredibly rare, making Zack’s story all the more important.

