8 uveitis symptoms and treatment options

If you experience a dull ache in or around the eye, blurred vision or an increased sensitivity to light, you could be at risk of uveitis. Uveitis is the name given to inflammation of the middle layer of the eye, called the uvea. It may occur at any age and if it not treated promptly may cause significant problems including loss of vision, so if you have any concerns about your eye health get it checked out by your doctor.
Family GP Dr Roger Henderson looks at uveitis causes, symptoms and treatment options:
What is uveitis?
Uveitis is the general term given to inflammation of the middle part of the eye called the uvea or uveal tract. The uveal tract is made up of the iris that gives eyes their colour, the ciliary body which sits behind the iris and helps the eyes to focus, and the choroid which is the tissue between the retina and the sclera, which helps absorb excess light.
The term uveitis covers a variety of types of this eye problem depending on the part of the uvea that is affected. Uveitis is more common in people aged 20 to 59 but can occur at any age, and it has been estimated that between two and five people in every 100,000 suffer from it every year in the UK. The most common types of uveitis include the following:
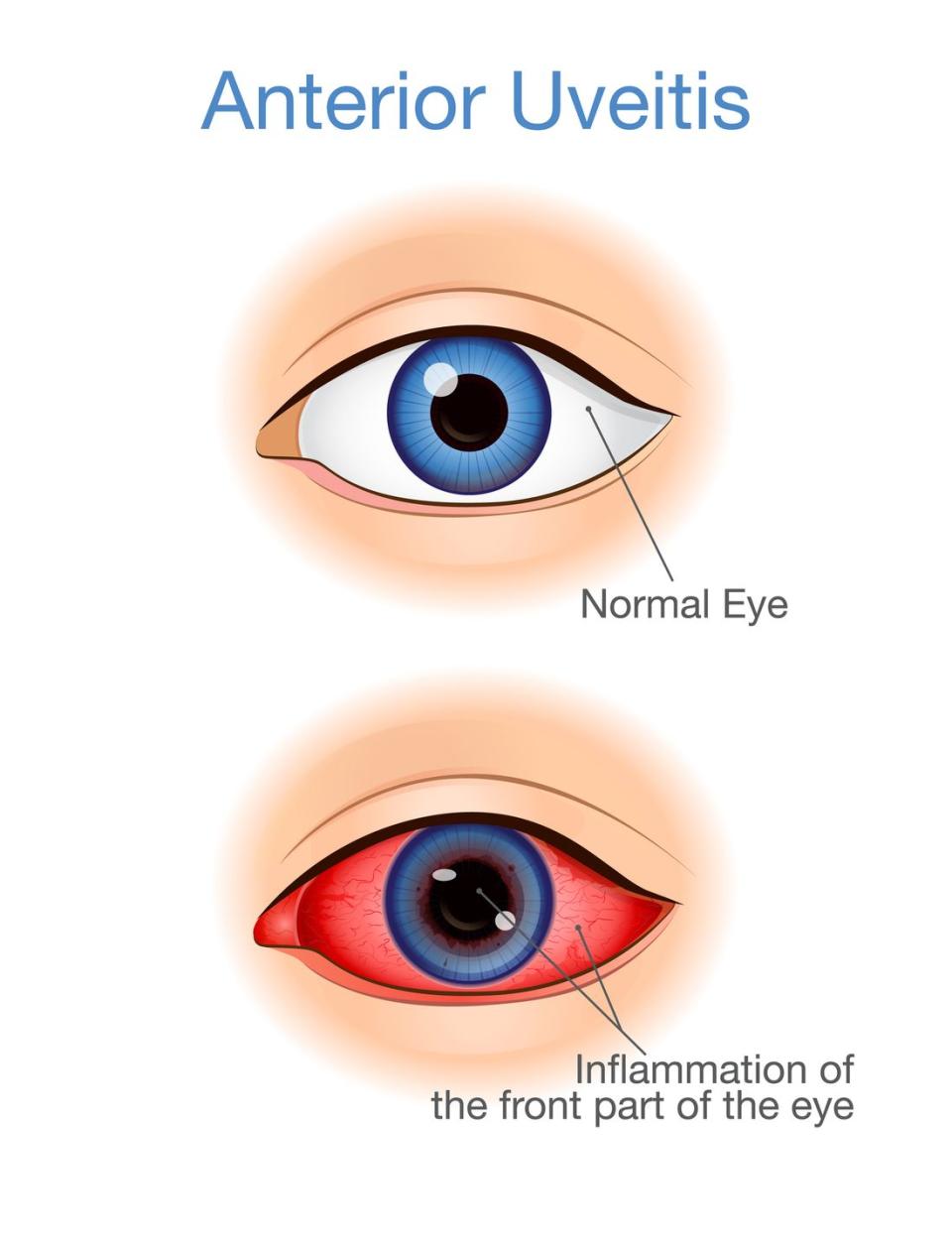
• Anterior Uveitis
Anterior uveitis is the most common type of uveitis and accounts for most cases in the UK. It refers to inflammation of the iris and can be divided into acute types (the commonest form, usually lasting less than six weeks) and chronic types that last longer than three months. It is typically the most painful form of uveitis.
• Intermediate uveitis
Intermediate uveitis affects the middle part of the eye, around and behind the ciliary body. It can be linked to certain medical conditions, such as sarcoidosis.
• Posterior uveitis
Posterior uveitis affects the back of the eye around the retina. It is sometimes called chorioretinitis and is the least common form.
• Panuveitis
When inflammation affects both the front and back of the eye it is known as panuveitis, and is the most serious of all forms of uveitis. Panuveitis can cause severe damage to the retina, and is often caused by Behcet’s disease.
Although anterior uveitis is the most common type, intermediate, posterior and panuveitis forms that are most likely to cause problems with vision.
What causes uveitis?
In around half of all uveitis cases, no obvious cause is ever found even after all investigations have been done – this is known as idiopathic uveitis. When a cause is found, the main ones are:
Autoimmune and inflammatory conditions: in autoimmune diseases (such as rheumatoid arthritis) the immune system attacks the body rather than protecting it, and this then in turn triggers uveitis. Inflammatory conditions such as inflammatory bowel disease, sarcoidosis and psoriasis may also make it more likely that uveitis can occur.
Infective: infections may cause inflammation of the eyes and there are many possible types of infection that can be involved but toxoplasmosis is the commonest infection found in anterior uveitis. Other examples of infection causing it include TB, herpes and gonorrhoea.
Eye injuries: any eye injury has the potential to cause inflammation and uveitis but in general the more severe the injury, the greater the risk.
Cancer-linked: cancers that can be linked with the condition include lymphomas, leukaemias and malignant melanomas of the eye.
8 common uveitis symptoms
Symptoms vary depending on the type of uveitis present, and can develop suddenly or gradually. One or both eyes may be affected but in some cases the symptoms may be so mild they are not noticed, or dismissed as being insignificant. If present, uveitis symptoms include the following:
1. Eye pain
This is most common in anterior uveitis and is typically a dull ache in or around the eye, which may be worse when trying to focus the vision on something.
2. Redness of the eye
Redness of the eye can be a uveitis symptom.
3. Sensitivity to light
Sensitivity to light (photophobia) can be a uveitis symptom, so looking at bright lights becomes uncomfortable or painful.
4. Blurred vision
Blurred vision is more usual with intermediate and posterior uveitis, and there may also be some cloudiness of vision and an inability to see objects at the side of your visual field (out of the corner of your eye).
5. Floaters
These are small shapes that move across the vision, typically appearing as dark shapes that ‘float’ in the eyesight and are more commonly seen when looking at a bright background.
6. Headaches
Headache can be a uveitis symptom.
7. Watery eyes
Watery eyes can be a uveitis symptom.
8. Change in shape
A change in shape of the pupil of the eye can be a uveitis symptom.
⚠️Some uveitis symptoms can be less obvious, making it more difficult to diagnose. If uveitis is not treated promptly it may cause significant problems including loss of vision, so if you have any concerns about your eye health make an urgent appointment with your GP.
Uveitis diagnosis
Uveitis is normally diagnosed from the symptoms, with a doctor taking a detailed history and then doing a comprehensive examination of the eyes including using a microscope called a slit-lamp designed for eye examination.
Further tests may then be required depending on the symptoms and their severity, the most common of these being eye photographs and scans – which may include an optical coherence tomogram (OCT) - blood tests, and chest X-rays to rule out other illnesses that may be causing the uveitis.
Uveitis treatment
The sooner uveitis is treated the more successful treatment is likely to be. The aim of any treatment is to reduce the eye inflammation, and the choice of treatment depends on knowing the underlying cause if at all possible. Any infection, autoimmune disease or inflammatory condition needs to be treated as they normally would.
✔️ Steroids
The mainstay of treatment is steroids, usually in the form of eye drops but which can also be given by mouth. For mild cases of uveitis, simple steroid drops may be all that is required (such as dexamethasone or prednisolone) but these are usually prescribed by an eye specialist. There are potential risks if these drops are used inappropriately and for too long, such as the development of cataracts or glaucoma. (Some people with recurrent uveitis learn to recognise the early symptoms and are prescribed drops to keep in reserve and start at the first signs of their uveitis starting).
If the uveitis is severe then steroids can be given by mouth or as an injection into the eye. These can be extremely effective but if used for more than a few weeks can have side effects such as an increased risk of infection, weight gain, mood changes and thinning of the bones and skin. Should steroids be needed long-term, other medication called immunosuppressants can be taken to reduce the amount of steroid required. Never stop steroids suddenly as you may develop serious ‘rebound’ effects of inflammation – always discuss with your doctor first.
✔️ Painkillers
To help relieve and reduce any pain associated with uveitis, wearing dark glasses and taking regular simple painkillers such as paracetamol can be effective.
✔️ Cycloplegic eye drops
Using a special type of eye drop called a cycloplegic can help reduce any pain associated with uveitis. These dilate the pupil of the eye and in doing so allow the inflamed iris part of the eye to relax and recover. While they are working they cause temporary blurred vision and difficulty in focusing because of their action on the pupil.
✔️ TNF alpha-blockers
New treatments are being developed for uveitis such as TNF alpha-blockers (such as infliximab) that can be prescribed by specialists.
✔️ Surgery
Eye surgery may also sometimes be needed to treat problems such as cataracts or glaucoma, or persistent floaters that are severely affecting vision.
Uveitis potential complications
Risk of uveitis complications is highest in people with intermediate or posterior uveitis, or in those who have had repeated episodes of uveitis. If it is left untreated or not treated quickly enough there is a risk of complications such as glaucoma (raised pressure in the eye) or even permanent loss of vision.
Other possible uveitis complications include:
Cataract formation.
Macula oedema (a build-up of fluid in the back of the eye).
Synechiae - Tissue bands forming between the iris and the lens.
Most cases of uveitis fortunately respond well to treatment and do not cause long-term complications.
People with frequent or chronic uveitis are usually kept under long-term review with an eye specialist, and have regular eye checks at hospital.
Last updated: 06-05-2021
You Might Also Like


