7 hormone-free contraceptive options explained by an expert

Hormone-free contraceptive options are on the rise, with the likes of apps such as Natural Cycles and copper-based Intrauterine Devices (IUDs) being opted for more than ever. Many cite not wanting to have their weight, sex drive, period or mood altered when choosing a non-hormonal method of protection against pregnancy, but, says Babylon GP, Dr Elise Dallas, it's worth asking yourself a few questions before ditching the pill entirely.
"I always remind patients that many hormonal contraception side effects, such as weight gain and mood changes can be caused by other things," says Dr Dallas. "Think about whether you're sure it's the contraception that’s causing you issues." She adds that hormonal methods of contraception are still a solid choice for some.
In fact, they can significantly improve the quality of life for women with acne and heavy, painful periods. "As a first step, I suggest discussing the issues that are most important to you when it comes to birth control (e.g. it’s impact on your period) with your doctor." It's totally normal for your contraception needs to change depending on where you’re at in life, she adds. So, what are the options out there?
What are the most popular non-hormonal contraceptive options?
1. Male condoms
What are they?
Probably the most familiar method of non-hormonal contraception, male condoms are thin latex sheaths that go over the penis during sex. They're a good option if you're dating or hooking up with new people, as they (and female condoms) are the only methods that also offer protection from STIs.

Pros and cons:
"They're really easy to use and you only need to use them when you have sex," says Sue Burchill, head of nursing at sexual health charity Brook. "They protect against sexually transmitted infections (STIs) as well as pregnancy. Plus, they are available for free from Brook services (for under 25s), some youth clinics, contraception and sexual health clinics and some GPs. You can also buy them at any time of day from supermarkets, vending machines in public toilets, petrol stations etc, even if you're under 16. They also come in different shapes, sizes, textures, colours and flavours which can make sex more fun."
Condoms are the only type of contraception that a man can use to control his own fertility, but they do also have some potential disadvantages. "Some people are allergic to the latex used in condoms. This is rare but if you or your partner is allergic, it's possible to use latex free polyurethane condoms," Sue adds. "Sometimes they can split or slip off – if this happens or you are worried you may need emergency contraception."
2. Female condoms
What is it? Female condoms, sometimes known as ‘femi-doms’, are similar to male condoms, except they’re worn internally, inside the vagina, instead of going over the penis.
Pros and cons:
Like their male counterparts, female condoms also protect you against STIs and pregnancy, and are available for free within many of the same services. You can also put them in before you have sex (up to eight hours before).
If they’re not used properly, however, female condoms can slip or get pushed up into the vagina - and again, if this happens, you might need to seek emergency contraception. "You need to make sure the penis goes into the condom and not between the condom and the vagina," advises Sue. It’s also worth noting that female condoms are not always available at every contraception and sexual health clinic and can be more expensive to buy than other condoms.
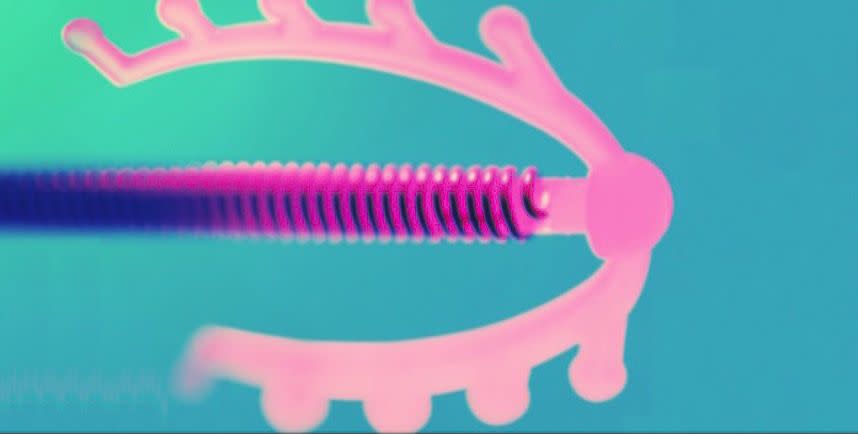
3. IUDs
What is it?
Intrauterine devices, or IUDs, are t-shaped plastic devices that contain copper, and stop an egg from implanting in your uterus. They need to be fitted by your doctor or nurse.
Pros and cons:
Copper-based IUDs provide a long-term solution that once fitted, can prevent pregnancy immediately, and for up to 10 years (depending on what type of IUD you go for). They don’t interrupt sex, or mess with your fertility, and, crucially, you don’t have to remember to pop a pill every day for it to be effective. "The IUD is not affected by vomiting, diarrhoea or other medicines like other methods of contraception," Sue notes - in fact, it can even be fitted as a method of emergency contraception.
This is not to say that the IUD has no potential pitfalls. "It doesn't protect against STIs, and your periods may be heavier, more painful or last longer," she adds. There are also several risks, although slim and unlikely, that come with fitting and using the IUD; for example, you may get an infection when it’s inserted, it can be be pushed out or displaced, and there is very minor chance of perforation of the uterus. If you do somehow get pregnant when you’re using one, there is also a small risk of ectopic pregnancy.
4. Cervical caps or diaphragms
What is it? These are dome-shaped devices which look similar, but diaphragms fit into the vagina and over the cervix, whilst caps need to be put onto the cervix directly. They need to be fitted by a professional on the first occasion, and used in conjunction with spermicide for maximum effectiveness.

Pros and cons:
"They can be put in before sex so they don't disturb the moment (you will need to add extra spermicide if you have sex more than three hours after putting it in)," says Sue. "They are not affected by any medicines that you take orally, and don't disturb your menstrual cycle" - although it is recommended that you do not use the diaphragm/cap during your period, so you will need to use an alternative method of contraception at this time.
And the downsides? As with pretty much all methods except condoms, they don’t provide protection against STIs, and they’re also not as effective at preventing pregnancy as other methods (around 92-96%, compared with 98% for male condoms, for instance). "They can take a little getting used to before you're confident using them," Sue admits, "Some women can develop the bladder infection cystitis when using diaphragms or caps – check with your doctor or nurse if you need further advice. Some people may be sensitive to latex or the chemical used in spermicide."
5. Sponges
What is it? This option is very much 'does what it says on the tin' – it's a sponge containing spermicide that you insert to help to prevent pregnancy. They’re a single use option, with a 30 hour maximum usage.
Pros and cons:
Sponges provide protection from pregnancy on a two-fold basis - the spermicide slows sperm down and stops them from heading towards the egg, and the sponge itself covers your cervix, to block them if they do get there. They are easy enough to use, but do require a little bit of prep: you have to wet the sponge to activate the spermicide, and then insert it, as far up as you find comfortable. They also need to be left in your vagina for at least six hours after having sex, so you have to remember to include this in your 30 hour calculation. It shouldn’t happen, but if the sponge breaks into pieces when you pull it out, you need to contact your doctor right away.
Once again, there’s no STI protection, and you can’t use them when you’re on your period, or have any form of vaginal bleeding, as this could increase your chances of getting toxic shock syndrome. They’re also not recommended for women who’ve had physical trauma in the area, or given birth, been through miscarriage or abortion recently. If you’re unsure, talk to a professional before making your purchase (because unlike many other options, sponges aren’t given out for free).
6. Natural family planning
What is it? Natural family planning, also called Fertility Awareness Methods (FAM) include apps like Natural Cycles, which work by monitoring your fertility signs, such as cervical secretions and basal body temperature, to find out when during the month you can have sex with a reduced risk of pregnancy. Because they're typically in the region of being 75% effective, the NHS advise this as a method for women who wouldn't find falling pregnant a significant problem.
A post shared by Natural Cycles (@naturalcycles) on Sep 26, 2017 at 12:51am PDT
Pros and cons:
It can be used to plan pregnancy as well as avoid pregnancy, if you’re thinking of starting and family – and if you’re not, it doesn't involve taking any hormones or other chemicals or using physical devices, like many other methods do. The NHS states that it’s up to 99% effective if the method is followed precisely - but you need proper teaching about the indicators, and because it can be tricky to master, mistakes happen, so it’s generally around 75% mark instead.
You’ll still need to consider protection from STIs, and use a different form of contraception if you want to have sex during your fertile times. "You need to keep daily records, and some things such as illness or stress can make results difficult to interpret," says Sue. "It can take longer to recognise your fertility indicators if you have an irregular cycle, or have stopped using hormonal contraception. It demands a high level of commitment from both partners."
7. Tubular occlusion
What is it? Tubular occlusion, or female sterilisation, is a surgical method of contraception that involves using clips or rings to block your fallopian tubes. It is thought to be more than 99% effective, and doesn’t effect hormone levels. You’ll still get your period if you have it done too (sorry).
Pros and cons:
If you’re certain that sterilisation is the right option for you, it means that you no longer have to worry about pregnancy (although the same can’t be said for STI’s, which you’ll still need protection from). There shouldn’t be any impact on your sex drive, and rarely has any other long-term effects on your health.
However, as with any operation, there are potential complications, including internal bleeding, infection, or damage to your other organs. The chance of sterilisation failing is around in 1 in 200, but it can happen, and if it does occur, there’s a higher chance of the pregnancy being ectopic. Surgeons are generally more willing to carry out sterilisation on women who are over 30 and have already had children, but you can request it whatever your circumstances. It’s likely you’ll be referred to counselling before making your final decision, because of the permanent nature of the choice that you’re making.
Like this article? Sign up to our newsletter to get more articles like this delivered straight to your inbox.
You Might Also Like

